The problem of joint diseases is always relevant. After forty years, about a third of all people begin to experience pain when moving, and after fifty, more than half of the population begins to experience pain. The gradual destruction of cartilage, ligaments, bones and soft tissues around the joints is called by doctors the general term "osteoarthritis".
How can this condition be prevented? And what treatments will help relieve pain when the disease has already developed? To answer these questions, you first need to understand the difference between arthritis and arthrosis - the most common joint pathologies.
What is arthritis?
What is the main difference between arthritis and arthrosis can be seen from the names: acute, sudden illnesses end with "-itis"; with "-from" – diseases with a slow course, chronic processes.
Arthritis is an inflammatory lesion of the joints that occurs due to a malfunction of the immune system due to infection (for example, sore throat or otitis media), trauma, metabolic disorders, hypothermia, stress or other reasons (even autoimmune).
The first signs appear like this:
- sharp pain in one or more joints (often not only during movement), especially early in the morning;
- enlargement, swelling, edema, redness of the sore joint;
- a noticeable increase in temperature at the site of inflammation.
Inflammatory processes caused by arthritis can affect the entire body. In this case, the patient feels a high temperature, chills, loses strength, and may experience inflammation of other organs (eyes, genitourinary system, even the heart, lungs, liver and kidneys).
Arthritis has several dozen forms. The most common of them are:
- rheumatism– inflammation of the connective tissue of large and medium-sized joints that occurs after infections;
- rheumatoid arthritis– an autoimmune slow process that symmetrically affects several joints at once; causes the appearance of "nodules", pain, loss of mobility; can cause inflammation of many organs;
- gout– caused by the accumulation of uric acid in the blood and salts in the joints; most often begins with sharp pain in the joint of the big toe;
- reactive arthritis– occurs against the background of damage to the body by infections (chlamydia, streptococci, etc. );
- infectious arthritis– begins due to bacterial infection of the joint itself.
What is arthrosis?
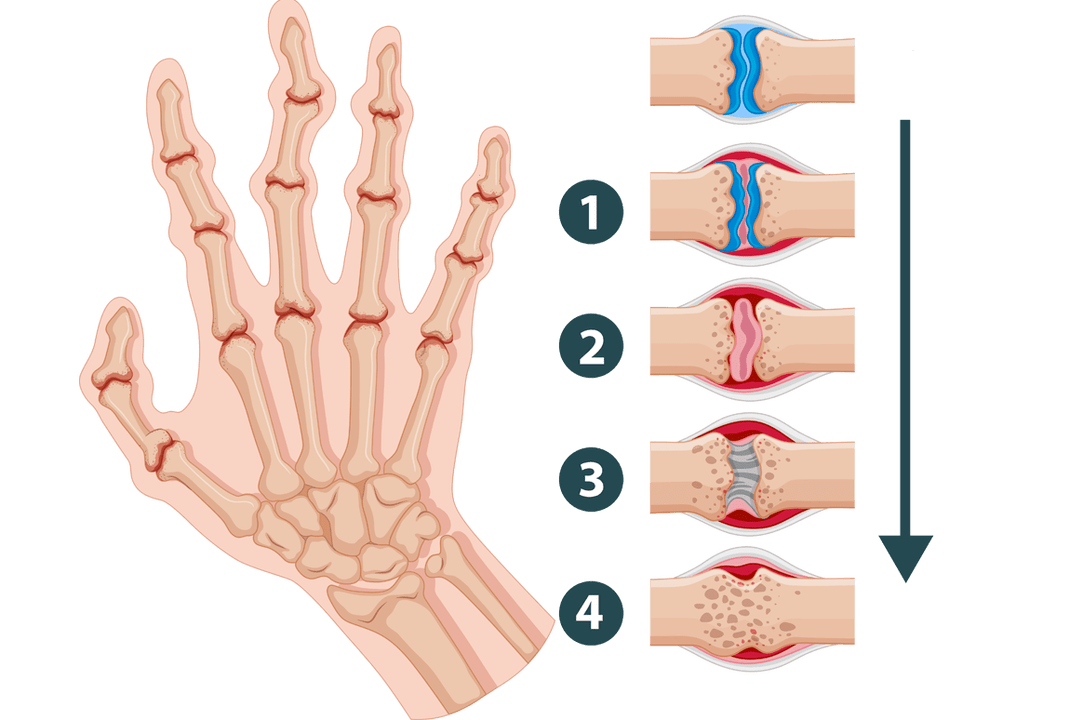
Unlike arthritis, arthrosis is not accompanied by inflammatory processes. It provokes poor circulation in the joint, which causes the cartilaginous parts to begin to dry out.
Arthrosis is a disease that deforms and destroys joint tissue. With it, the connecting layers are dehydrated, become thinner and "worn out". The bones begin to touch each other, which causes pain and makes it difficult for a person to move.
Signs of arthrosis of joints are:
- after a long period of immobility (for example, a night's rest), the joint "freezes", but then quickly develops when activity resumes;
- the operation of the joint is accompanied by strange sounds (clicking, crunching, grinding);
- physical activity causes pain.
What are the differences between arthritis and arthrosis?
Both of these diseases affect the joints. But they are caused by different reasons, proceed differently and can lead to very different consequences. Only correct diagnosis, based on the difference between arthritis and arthrosis, can prevent irreparable harm to the body.
It takes time for cartilage tissue degeneration to develop sufficiently and bone deformation to begin. Therefore, chronic arthrosis usually manifests itself in old age (after 60 years, less often after 50). The most susceptible to changes are the joints that constantly work under load: the fingers of musicians, the knees of athletes and loaders, the ankles of people who walk a lot or work while standing, etc.
In contrast, arthritis can occur even in a child. The inflammatory process causes pathology of the synovial membrane, saturated with blood vessels, and joint fluid (whereas with arthrosis it is simply produced in insufficient quantities). Unfortunately, almost every fifth case of disability in the world is caused by various forms and complications of arthritis.
Inflammation can affect not only joints, but also other tissues with active blood circulation: blood vessels and heart, lungs, abdominal organs, eyes, urinary system, etc. On the other hand, arthrosis is limited by local mechanical damage to bones and the formation of osteophytes in areas of joint deformation. Although in late stages and advanced forms, the disease can also lead to disability, completely immobilizing a person’s limbs.
How do arthritis and arthrosis manifest?

Let’s compare the external manifestations to clearly explain the difference between the symptoms of arthritis and arthrosis.
- Pain. In the initial stages of arthrosis (which lasts for years), joint pain occurs during physical activity and goes away after rest. It is rarely sharp and strong. Even as the disease develops, when pain can appear even with small movements and even at rest, it is usually enough to give the body a comfortable position for the pain to subside. With arthritis, the patient is bothered by sharp pain attacks of great strength, which can only be extinguished by special medications. A characteristic symptom is pain during rest, especially early in the morning.
- Clicking, grinding, crunching of joints. In joints affected by arthrosis, the cartilage layers are destroyed. They stop protecting the heads of the bones from contact with each other. Therefore, when moving, the bones touch and rub, producing rough, dry sounds. The more the disease progresses, the stronger and louder the joints click. Arthritis is usually not accompanied by such symptoms.
- Deformation of the joint and surrounding tissues. Developing arthrosis over time causes a change in the shape of the bones: their heads begin to crumble and wear out, and osteophytes may appear. Sometimes in the acute stages there is swelling and aching pain, but these symptoms are not permanent. But a joint affected by arthritis becomes inflamed and swollen. Swelling forms and compactions occur. The skin turns red and becomes hot.
- Limited mobility. Osteoarthritis causes stiffness in a specific joint that goes away with movement. At deeper stages, stiffness increases, the amplitude of flexion decreases, ultimately leading to immobility. With arthritis, you may feel stiff throughout your body, and attempts to move will cause sharp pain.
- Changes in blood composition. Arthrosis is not an inflammatory disease, so it is not reflected in the analysis. Arthritis causes a significant increase in the erythrocyte sedimentation rate, which indicates an active infectious and inflammatory process.
Thus, symptoms of arthrosis in the early stages can rarely cause severe anxiety and discomfort. This leads to a careless attitude and late diagnosis of the disease, which means it complicates further treatment.
Causes of osteoarthritis
There are several factors that increase the risk of pathological changes in the joints and surrounding tissues: constant overload, imbalance of the immune and hormonal systems, poor physical shape. Therefore, to prevent illness, you need to regularly follow these recommendations:
- Maintain moderate physical activity through simple exercises, walking, swimming, etc. This will help you get rid of excess weight, improve blood circulation, strengthen muscles - and thereby relieve stress on your joints.
- Try to eat healthy foods. Fatty foods, red meat, and alcohol can be harmful. On the contrary, seafood, fruits and vegetables, and dishes containing cartilage and gelatin will be beneficial for the body. It is important to drink a lot of clean water (2-3 liters per day).
- Choose suitable clothes and shoes: comfortable heels, warm enough, not restricting movement.
- If possible, avoid stress, disruptions and other "shocks" to the body.
However, if a person has already been diagnosed with arthritis or arthrosis, before performing even such simple actions, you should consult a doctor. In some cases, conventional prevention can also cause harm and worsen the condition.
But how are arthritis and arthrosis treated? What is the difference? The causes of these pathologies differ: immune processes, fighting infection in the first case versus malnutrition of cartilage in the second. Therefore, the ways to deal with them will be different. To choose the right course of action, you must first make an accurate diagnosis.
To do this, it is best to undergo radiography and MRI in combination with laboratory blood and urine tests. After studying the results, the doctor will prescribe appropriate recommendations.
Arthritis treatment
If the acute form of the disease is caused by an infection, then it can be cured with antibiotics. But in this case, it is important to accurately select the drug: it is necessary to neutralize pathogenic bacteria before the pathology of the joint becomes irreversible. The course is supplemented with anti-inflammatory and immune-supporting medications.
In the case of chronic arthritis (for example, rheumatoid), treatment must be carried out regularly throughout life. The most commonly used are corticosteroids, cytostatics and modern biological products. These are quite powerful drugs, so to ensure that they do not cause harm to the body, the correct calculation of dosages, frequency and duration of use is critical.
For severe pain, your doctor may also prescribe a course of analgesics. And accompanying methods of support are necessarily recommended: diet, physical therapy, and a course of physical therapy. If the inflammation has spread to other organs, the patient must be referred for additional specialized examinations.
Treatment of arthrosis
Modern methods make it possible to almost completely get rid of the manifestations of the disease if the diagnosis was made at an early stage and the patient’s age does not reach forty years. To do this, in addition to standard monitoring of stress on the joint and a course of medications (they initiate regeneration, restore nutrition and hydration of the cartilage), the patient may be prescribed mud wraps, electrophoresis and acoustic therapy (which affects the affected tissue with low-frequency sounds).
In older people or in advanced forms, arthrosis cannot be completely cured, although it is possible to achieve a significant improvement in the condition and slow down the destructive processes in the joint. This requires strict adherence to the doctor’s recommendations: regular use of medications (for example, chondroprotectors), maintaining a healthy lifestyle, timely completion of prescribed procedures, monitoring joint load.
In arthrosis, the main attention is paid to the restoration of the cartilage layer. If there are concomitant symptoms of inflammatory processes, antibiotics or corticosteroids may be prescribed to relieve the acute stage and move on to the main treatment regimen. In some severe cases, surgery and even implantation of an artificial joint may be required.
























